A Comprehensive Guide to Type 2 Diabetes: Symptoms, Causes, and Treatments
By David Jackson
Type 2 Diabetes is a complex medical condition. Our guide introduces the topic.
Introduction
Type 2 diabetes is a chronic condition that affects the way your body processes glucose (sugar), leading to high blood sugar levels. It’s the most common form of diabetes, accounting for around 90-95% of all diagnosed cases. In this comprehensive guide, we’ll explore the symptoms, causes, and treatments for Type 2 diabetes, as well as strategies for managing the condition and reducing the risk of complications.
Symptoms of Type 2 Diabetes
Type 2 diabetes can develop slowly, and many people may not notice any symptoms at first. However, common symptoms include:
- Increased thirst and frequent urination
- Increased hunger
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Areas of darkened skin
If you experience any of these symptoms, it’s important to consult with a healthcare professional for proper diagnosis and treatment.
Causes of Type 2 Diabetes
Type 2 diabetes is primarily caused by a combination of insulin resistance and insufficient insulin production. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. In Type 2 diabetes, the body becomes resistant to insulin, and the pancreas cannot produce enough insulin to overcome this resistance.
Several factors can increase your risk of developing Type 2 diabetes, including:
- Family history
- Obesity or being overweight
- Physical inactivity
- High blood pressure
- High cholesterol
- A history of gestational diabetes or giving birth to a baby weighing more than 9 pounds
- Ethnicity (African Americans, Hispanic Americans, Native Americans, Asian Americans, and Pacific Islanders are at higher risk)
Diagnosis and Treatment
To diagnose Type 2 diabetes, healthcare professionals may use blood tests such as fasting plasma glucose, oral glucose tolerance test, or A1C test. Once diagnosed, treatment for Type 2 diabetes typically involves lifestyle changes, oral medications, and possibly insulin injections.
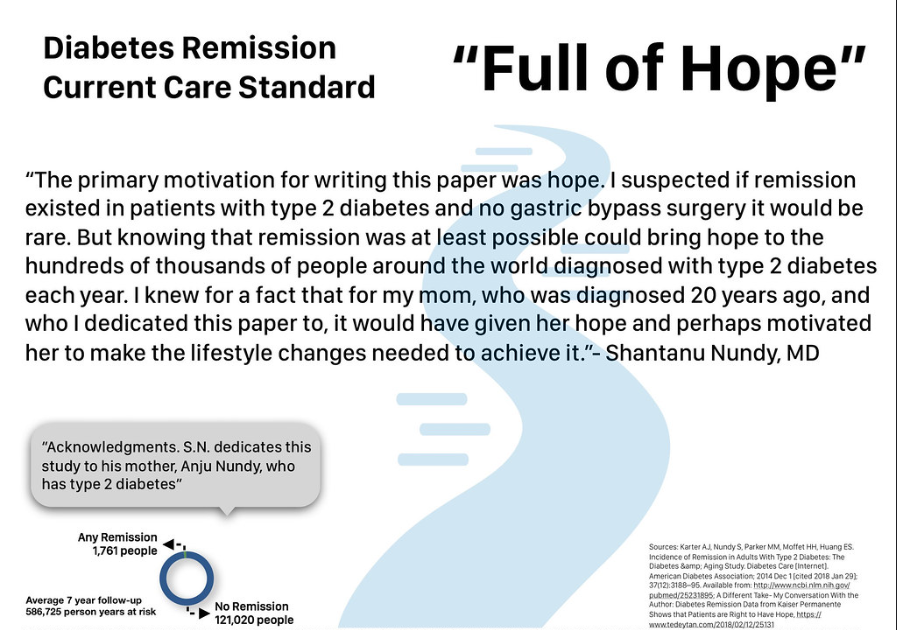
Figure 1: A hopefull message for people with Type2 Diabetes
Lifestyle Changes
Lifestyle changes are crucial in managing Type 2 diabetes and may include:
- Following a healthy, balanced diet that’s low in added sugars and high in fiber
- Regular physical activity, such as walking, swimming, or cycling
- Losing weight, if necessary
- Quitting smoking
- Limiting alcohol consumption
Medications
Oral medications for Type 2 diabetes work in various ways to help lower blood sugar levels. Some common medications include:
- Metformin: Helps lower blood sugar by reducing the amount of glucose produced by the liver and increasing insulin sensitivity
- Sulfonylureas: Stimulate the pancreas to produce more insulin
- DPP-4 inhibitors: Help lower blood sugar levels by increasing insulin production and reducing glucose production in the liver
- GLP-1 receptor agonists: Slow digestion and help lower blood sugar levels by increasing insulin production
Insulin Therapy
Some people with Type 2 diabetes may require insulin therapy if their blood sugar levels are not well controlled with oral medications. Insulin can be injected using a syringe, insulin pen, or insulin pump.
Managing Type 2 Diabetes
Proper management of Type 2 diabetes is crucial to reduce the risk of complications and improve quality of life. This may involve:
- Regularly monitoring blood sugar levels
- Taking medications as prescribed
- Following a diabetes meal plan and making healthy food choices
- Engaging in regular physical activity
- Maintaining a healthy weight
- Keeping up with routine medical appointments and screenings
Reducing the Risk of Complications
Long-term complications of Type 2 diabetes can affect various parts of the body, including the eyes, kidneys, nerves, heart, and blood vessels. To reduce the risk of these complications, it’s important to:
- Keep blood sugar levels within your target range
- Manage blood pressure and cholesterol levels
- Attend regular check-ups and screenings, such as eye exams, foot exams, and kidney function tests
- Practice good foot care, including daily inspection, washing, and moisturizing to prevent infections and ulcers
- Manage stress and prioritize mental health
Support and Resources
Living with Type 2 diabetes can be challenging, but you don’t have to face it alone. There are numerous resources and support networks available to help you manage the condition, including:
- Diabetes education programs and support groups
- Online communities and forums where people with diabetes can share experiences, tips, and advice
- Healthcare professionals, such as dietitians, diabetes educators, and endocrinologists, who can provide guidance and support tailored to your individual needs
Conclusion
Type 2 diabetes is a complex condition that requires ongoing management and care. By understanding the symptoms, causes, and treatments, you can take control of your health and reduce the risk of complications. With the right support and resources, living with Type 2 diabetes can be manageable, allowing you to lead a healthy, fulfilling life.