Unveiling the Mystery of Insulin for Type 2 Diabetes
By Type2 Advice
Understanding and Using Insulin in the Context of Type 2 Diabetes
Imagine being able to control your blood sugar levels with a simple injection. Imagine being able to eat your favorite foods without worrying about the consequences. Imagine being able to live a longer and healthier life with diabetes.
This is not a fantasy. This is what insulin can do for you.
Insulin is a hormone that helps your body use glucose, the sugar that comes from the food you eat and gives you energy. Without insulin, glucose builds up in your blood and causes serious damage to your organs and tissues.
For people with Type 1 Diabetes, insulin is a necessity. Their pancreas does not produce any insulin at all, so they need to inject it several times a day to survive.
For people with Type 2 Diabetes, insulin is an option. Their pancreas still produces some insulin, but not enough or not effective enough to keep their blood sugar levels in check. They may be able to manage their diabetes with oral medications, diet, and exercise, but sometimes these are not enough. That’s when insulin comes in handy.
Insulin can help people with Type 2 Diabetes lower their blood sugar levels and prevent or delay the complications of diabetes, such as nerve damage, kidney damage, eye damage, heart disease, and stroke. Insulin can also help them achieve better blood sugar control than oral medications alone.
If you have been recently diagnosed with Type 2 Diabetes and insulin as a possible treatment option, this comprehensive guide is for you. It will explain what insulin is, how it works in your body, how to use it safely and effectively, and how to overcome some of the common challenges and fears associated with it.
By the end of this guide, you will have a better understanding of insulin and how it can help you manage your diabetes. You will also feel more confident and empowered to take charge of your health and well-being.
Introduction to Insulin and Its Biological Role
What is Insulin?
Insulin is a hormone that is produced by the pancreas, an organ located behind the stomach. Hormones are chemical messengers that travel through the bloodstream and affect various processes in the body.
Insulin has a crucial role in our body’s metabolic process, particularly in the regulation of glucose. Glucose is a type of sugar that comes from the carbohydrates we eat, such as bread, rice, pasta, fruits, and sweets. Glucose is the main source of energy for all the cells in our body.
Insulin and Glucose Metabolism
The relationship between insulin and glucose is quite straightforward. When we eat, our blood glucose levels rise and signal the pancreas to release insulin into the bloodstream. Insulin then acts like a key that unlocks the cells and allows glucose to enter them. This lowers the blood glucose levels and provides energy to the cells.
This process is illustrated by the following diagram:
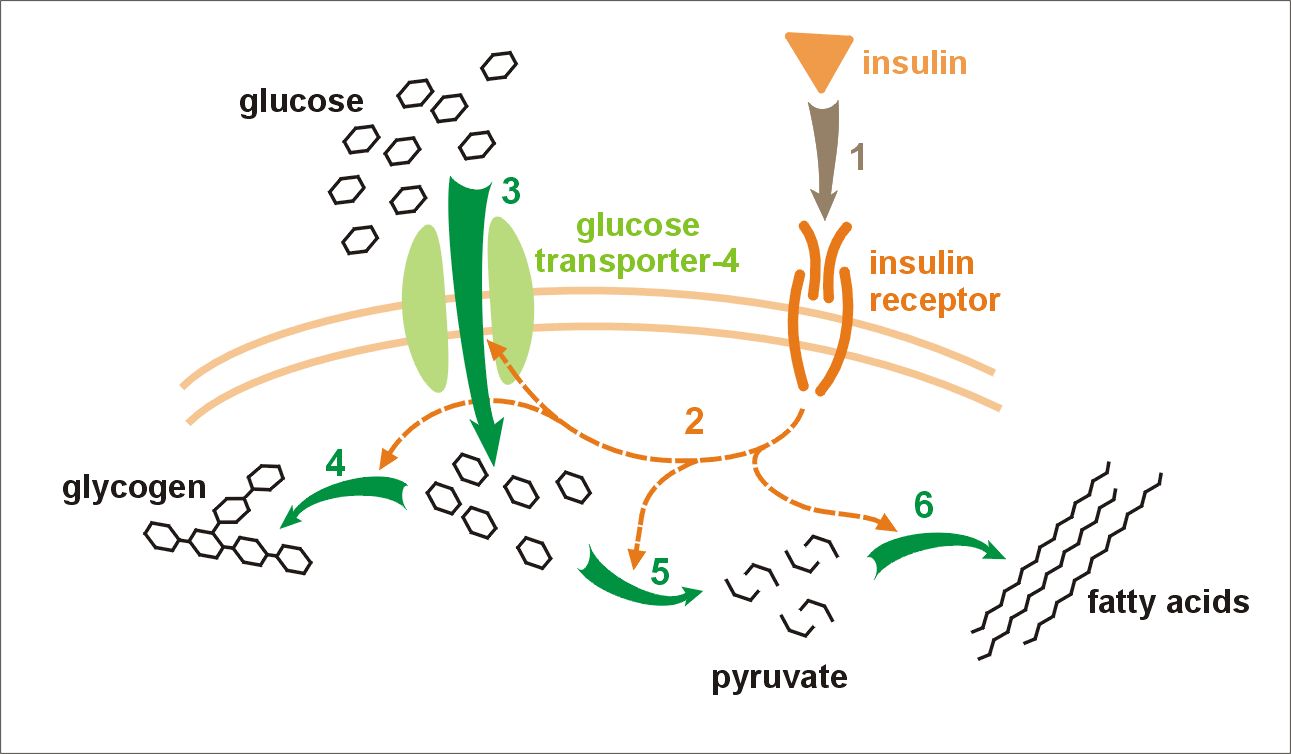
Figure 1: Insulin glucose metabolism
In a healthy person, this process keeps the blood glucose levels within a normal range throughout the day. However, in a person with diabetes, this process does not work properly.
Insulin Dysfunction in Type 2 Diabetes
In Type 2 Diabetes, either the pancreas does not produce enough insulin or the cells become resistant to its effects. This causes high blood glucose levels (hyperglycemia), which can lead to various complications over time.
There are several factors that can contribute to the development of Type 2 Diabetes, such as genetics, age, obesity, physical inactivity, poor diet, stress, and certain medications. Type 2 Diabetes usually develops gradually and may not cause any symptoms at first. However, some common signs and symptoms include:
- Increased thirst and urination
- Increased hunger
- Fatigue
- Blurred vision
- Slow healing of wounds
- Frequent infections
- Tingling or numbness in the hands or feet
If you experience any of these symptoms or have a family history of diabetes, you should see your doctor for a blood test to check your blood glucose levels. The sooner you diagnose and treat your diabetes, the better your chances of avoiding complications.
Insulin’s Role in Managing Type 2 Diabetes
The Need for Insulin Therapy
For those with Type 2 Diabetes, insulin therapy helps fill the gap caused by the body’s inability to produce or use insulin efficiently. By injecting insulin into the body, people with Type 2 Diabetes can lower their blood glucose levels and prevent or delay the onset of complications.
Insulin therapy is not a sign of failure or weakness. It is a sign of taking control of your health and well-being. Many people with Type 2 Diabetes benefit from starting insulin therapy early in their disease course, as this can help preserve their pancreas function and prevent further deterioration.
Your doctor will help you decide if and when you need to start insulin therapy based on several factors, such as:
- Your blood glucose levels
- Your symptoms
- Your treatment goals
- Your lifestyle
- Your preferences
Different Types of Insulin and How to Use Them
Fast-Acting Insulin
This insulin starts working super fast, around 15 minutes after you take it. It works the most after 1 hour and lasts for about 2 to 4 hours. You would normally take it before you eat to balance out the sugar that gets into your blood from your food. Some types of this insulin include Humalog, NovoLog, Apidra, Fiasp, Lyumjev, and Afrezza which you can inhale.
Short-Acting Insulin
This insulin gets into your blood around 30 minutes after you take it. It works the most between 2 to 3 hours after you take it and lasts for around 3 to 6 hours. Just like the fast-acting insulin, you would take this before you eat to balance the sugar from your food. The types of this insulin are Humulin R and Novolin R.
Medium-Acting Insulin
This insulin starts to work a couple of hours after you take it and lasts between 12 to 18 hours. You would usually take this once or twice a day to help control your sugar levels throughout the day and night. Some examples are Humulin N and Novolin N.
Long-Acting Insulin
This insulin takes a few hours to start working but then it works steadily for about 24 hours. You’d normally take this once a day to help keep your sugar levels steady all day and all night. Some types of this insulin include Lantus, Levemir, Toujeo, Basaglar, Tresiba, and Semglee.
Mixed Insulin
This is a mix of two types of insulin. One part works at meal times and the other part works between meals. You would usually take this twice a day before breakfast and dinner. This helps keep your sugar levels steady both at mealtimes and in between. Some types of this insulin are Humalog Mix50/50, Humalog Mix75/25, NovoLog Mix70/30, Humulin 70/30, and Novolin 70/30. Complicated names but they mean a lot to both you and your Dr
Your doctor will help you pick the best type of insulin for you. They will think about your usual sugar levels, your lifestyle, what you like, and your goals. You will also have to check your sugar levels regularly and change how much insulin you take based on the results.
Figure 2: An Insulin Word Cloud
How to Administer Insulin
Modes of Insulin Administration
Insulin is typically injected beneath the skin (subcutaneously). There are various tools used for this purpose, including:
Syringes:
The most common way of injecting insulin. They allow doses to be meticulously adjusted and mixed if more than one type of insulin is needed. Syringes come in various sizes to suit different insulin requirements. A new needle must be attached each time you use a syringe.
Insulin pens:
These pen-like devices come in reusable and disposable forms. Reusable pens have replaceable cartridges, while disposable pens are pre-filled with insulin and disposed of when empty. Pens provide a more convenient and discreet method of insulin administration, letting you easily dial up your dose and inject with one hand. A new pen needle must be attached each time you use an insulin pen.
Insulin pumps:
These small, computerized devices deliver a continuous stream of insulin via a thin tube attached to a needle or cannula under your skin. They mimic the function of a healthy pancreas, delivering both a basal rate (the amount of insulin given per hour) and bolus doses (mealtime or correctional insulin given at once). Insulin pumps offer more flexibility and discretion than injections, allowing you to quickly adjust your dose according to your needs. The infusion set must be changed every two to three days, or as instructed by your doctor.
The choice of device will depend on a variety of factors, including comfort, convenience, cost, and lifestyle. Your doctor and diabetes educator will assist you in choosing and using the most suitable device for you.
Insulin Injection Sites
The abdomen, thighs, buttocks, and arms are common sites for insulin injections. It’s recommended to rotate the injection site to avoid fatty lumps under the skin which can interfere with insulin absorption. Proper technique and hygiene during administration are crucial.
To inject insulin using a syringe or a pen device, you will need to follow these steps:
- Wash your hands with soap and water.
- Check the expiration date and appearance of your insulin vial or pen. Do not use it if it is expired, cloudy, discolored, or contains particles.
- If you are using a vial, gently roll it between your palms to mix it (if it is premixed) or warm it up (if it is cold). Do not shake it vigorously as this can create air bubbles that can affect your dose.
- If you are using a pen device, attach a new needle and prime it by dialing up two units of insulin and pressing the plunger until a drop of insulin appears at the tip of the needle.
- Choose an injection site that is clean and dry. Pinch up some skin and insert the needle at a 90-degree angle (or a 45-degree angle if you are thin or injecting into a muscular area). Push the plunger down slowly until all the insulin is injected.
- Pull out the needle quickly and gently press on the injection site with a cotton ball or gauze for a few seconds. Do not rub or massage the area as this can speed up the absorption of the insulin and cause low blood glucose levels (hypoglycemia).
- Dispose of your used needle in a sharps container or another safe container.
To inject insulin using an insulin pump, you will need to follow these steps:
- Wash your hands with soap and water.
- Check your pump’s battery level and reservoir level. Replace them if they are low.
- Fill your pump’s reservoir with your prescribed type of insulin using a syringe.
- Attach your infusion set (a thin tube with a needle or cannula at one end) to your pump’s reservoir.
- Choose an infusion site that is clean and dry. Insert the needle or cannula under your skin using an insertion device or by hand. Secure it with tape or an adhesive patch.
- Connect your infusion set’s tubing to your pump’s reservoir.
- Program your pump’s basal rate (the amount of background insulin delivered per hour) and bolus doses (the amount of mealtime or correctional insulin delivered at once) according to your doctor’s instructions.
- Check your blood glucose levels regularly and adjust your pump settings accordingly.
You should change your infusion set every two to three days or as directed by your doctor. You should also check your infusion site regularly for signs of infection or irritation such as redness, swelling, pain, or pus.
Managing Potential Complications
Hypoglycemia
Hypoglycemia refers to the condition of having low blood sugar, which can be a side effect of insulin therapy. Symptoms can include feelings of weakness, shakiness, breaking out in a sweat, and confusion. Regularly monitoring your blood sugar, eating meals and snacks at regular times, and keeping a quick source of sugar handy can help you manage hypoglycemia.
Hypoglycemia can happen due to a number of reasons, such as:
- Taking too much insulin
- Missing or delaying meals
- Eating less than usual
- Doing more exercise than usual
- Drinking alcohol
If you need to treat hypoglycemia, you should consume 15 grams of a quick-acting carbohydrate. This could be glucose tablets, juice, or candy. After 15 minutes, check your blood sugar again. Keep doing this until your blood sugar returns to its normal range.
In severe cases of hypoglycemia, you might lose consciousness or have seizures. In these cases, you’ll need an injection of glucagon. This hormone quickly raises blood sugar levels. It’s a good idea to always keep a glucagon kit with you and make sure someone close to you knows how to use it in case of emergencies.
Hyperglycemia
Alternatively, high blood sugar, or hyperglycemia, can occur if too little insulin is administered or if the body’s insulin needs increase due to illness or stress. Regular blood glucose monitoring and communication with your healthcare provider are key to managing this.
Hyperglycemia can occur for various reasons, such as:
- Taking too little insulin
- Eating more than usual
- Being sick or stressed
- Having an infection or injury
Treating Hyperglycemia
Hyperglycemia, or high blood sugar, can be treated by taking additional doses of rapid or short-acting insulin as directed by your doctor. Additionally, drinking plenty of water can help your body flush out the excess glucose.
If you’re experiencing severe hyperglycemia with symptoms such as nausea, vomiting, abdominal pain, fruity-smelling breath, or difficulty breathing, it could be a sign of diabetic ketoacidosis (DKA). This is a serious condition that occurs when the body starts breaking down fat for energy, instead of glucose, resulting in the production of ketones that acidify the blood. If you suspect DKA, you should immediately seek medical attention. Treatment typically involves receiving intravenous fluids and insulin.
Conclusion
Using insulin for Type 2 Diabetes can be a daunting prospect, but it doesn’t have to be. With the right knowledge, guidance, and support, you can use insulin safely and effectively to manage your blood sugar levels and improve your quality of life.Insulin is not a sign of failure; it is a sign of empowerment. By embarking on the insulin journey, you are taking charge of your health and well-being.
Further Reading
- Diabetes.org: Insulin & Other Injectables
- Mayo Clinic: Diabetes management: How lifestyle, daily routine affect blood sugar
- NIDDK: Insulin, Medicines, & Other Diabetes Treatments
Scientific References
- Banting FG. The internal secretion of pancreas. J Lab Clin Med 1922;7:251–66.link
- American Diabetes Association. Standards of medical care in diabetes—2021 abridged for primary care providers. Clin Diabetes 2021;39:1–21.link
- Mayo Clinic Staff. Insulin therapy: Options for better diabetes control. Mayo Clinic link Accessed May 29th 2023.
- WebMD Medical Reference. Insulin for type 2 diabetes: when, why, and how. WebMD link Accessed May 29th 2023.
- National Institute of Diabetes and Digestive and Kidney Diseases. Low blood glucose (hypoglycemia). NIDDK link Accessed May 29th 2023.
- National Institute of Diabetes and Digestive and Kidney Diseases. High blood glucose (hyperglycemia). NIDDK link Accessed May 29th 2023.